Foraminal stenosis, a term often heard in the realm of spinal health, can be a perplexing issue for those who experience back or neck pain. In this article, we will delve into the intricate world of foraminal stenosis, exploring its causes, symptoms, and available treatments. By the end, you’ll have a better grasp of what this condition entails and whether surgery is the right path to take.
Unveiling the Anatomy: The Spinal Column
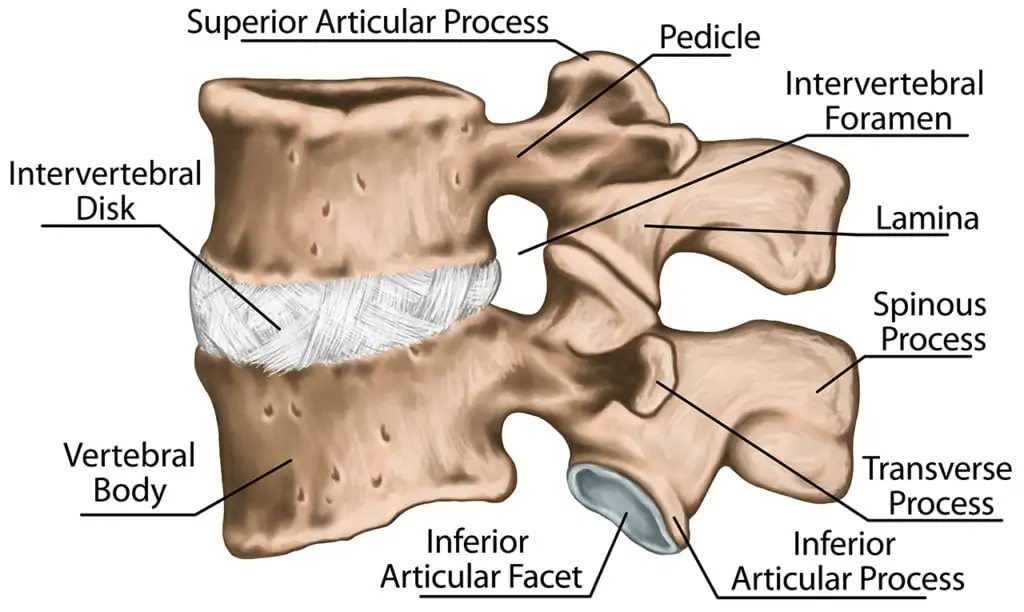
Before we dive into foraminal stenosis, it’s essential to comprehend the fundamentals of your spinal column. Your spine consists of a series of vertebrae, each separated by a cushioning disc that absorbs shock. Within this spinal column runs the spinal canal, a tunnel that houses the spinal cord—an intricate network of nerves that transmit commands to your muscles and relay sensory information to the brain.
The Exit Points: Foramina and Foraminal Stenosis
The spinal column isn’t just a simple structure; it has small holes, known as foramina, through which the nerves exit and branch off to various parts of the body. These foramina resemble tunnels branching out from the spinal canal. When your spine is healthy, the nerves can easily traverse these tunnels, efficiently transmitting sensory information from different parts of your body to the brain.
However, when the spine is not in optimal condition, this smooth flow of information can be disrupted, and that’s where foraminal stenosis comes into play.
Deciphering Foraminal Stenosis
Foraminal stenosis occurs when the spinal disc between the vertebrae bulges or when the spine joints develop arthritis, causing the foramen to narrow. This narrowing of the neural foramen results in the compression of spinal nerves, which can lead to various discomforting sensations.
Imagine a scenario where foraminal stenosis affects the lumbar spine, leading to nerve compression that extends down to your toes, causing numbness or tingling in your big toe. Similarly, foraminal stenosis in the cervical spine can result in sensations like tingling in your fingers or tightness in your biceps.
Recognizing the Symptoms
The symptoms of foraminal stenosis can vary based on the affected region of the spine:
Lumbar Stenosis:
- Muscle tightness
- Weakness
- Numbness
- Tingling
- Pain in the leg, buttocks, or feet
Cervical Stenosis:
- Muscle tightness
- Weakness
- Numbness
- Tingling
- Pain in the neck, shoulders, arms, or hands
Thoracic Stenosis:
- Muscle tightness
- Weakness
- Numbness
- Tingling
- Pain in the upper back or front of your body
These symptoms can intensify when you sneeze or cough, serving as potential indicators of foraminal stenosis.
Diagnosing Foraminal Stenosis
To diagnose foraminal stenosis, several methods are employed:
- Physical Examination: This involves assessing your pain levels, reflexes, movement, and muscle strength.
- Symptom Assessment: A comparison of your symptoms with those associated with foraminal stenosis.
- Diagnostic Imaging: X-rays, MRI scans, CT scans, and nerve conduction tests are used to examine whether the space between your spinal bones has narrowed.
Exploring Treatment Options
When it comes to treating foraminal stenosis, one of the options is surgery. However, it’s vital to understand that surgical intervention can have significant implications and potential side effects. Spinal fusion is often performed alongside surgery, but this should raise a red flag.
Why? Because adjacent segment disease (ASD) can occur, causing damage to the levels above and below the fused area. Moreover, relying solely on MRI findings for diagnosis can be misleading, as stenosis may not always be the direct cause of back pain.
Research indicates that physical therapy can be as effective as surgery in alleviating stenosis-related symptoms, making it a less invasive alternative. MVM Health’s platelet treatments are also worth considering, as they harness your body’s natural healing agents.
Is Foraminal Stenosis the Same as Spinal Stenosis?
A common point of confusion is the distinction between foraminal stenosis and spinal stenosis. Foraminal stenosis narrows the openings on the sides of the vertebrae through which spinal nerves exit, affecting specific areas of the body. On the other hand, spinal stenosis narrows the central spinal canal itself, impacting all the spinal nerves.
Both foraminal and spinal stenosis can result from issues like herniated discs, degenerative discs, or facet arthritis.
In conclusion, foraminal stenosis is a condition that can lead to discomfort and pain, but it’s crucial to explore all available treatment options and not rush into surgery without careful consideration.
Frequently Asked Questions
1. Can foraminal stenosis be cured without surgery?
Foraminal stenosis can often be managed without surgery, and alternative treatments like physical therapy and regenerative medicine should be considered before opting for surgery.
2. Is foraminal stenosis a common condition?
Foraminal stenosis is relatively common, especially among older adults, as it can be a result of age-related degeneration of the spine.
3. What causes foraminal stenosis?
Foraminal stenosis is primarily caused by factors like herniated discs, arthritis in the spine joints, or degenerative disc disease.
4. Are there any risks associated with surgical treatment for foraminal stenosis?
Yes, surgical treatment for foraminal stenosis can carry risks and potential complications, including adjacent segment disease (ASD).
5. How can I prevent foraminal stenosis?
While it may not always be preventable, maintaining a healthy lifestyle with regular exercise and good posture can help reduce the risk of developing spinal conditions like foraminal stenosis.
Don’t let foraminal stenosis leave you in the dark about your spinal health. Explore all available options, consult with medical professionals, and make informed decisions about your treatment journey.