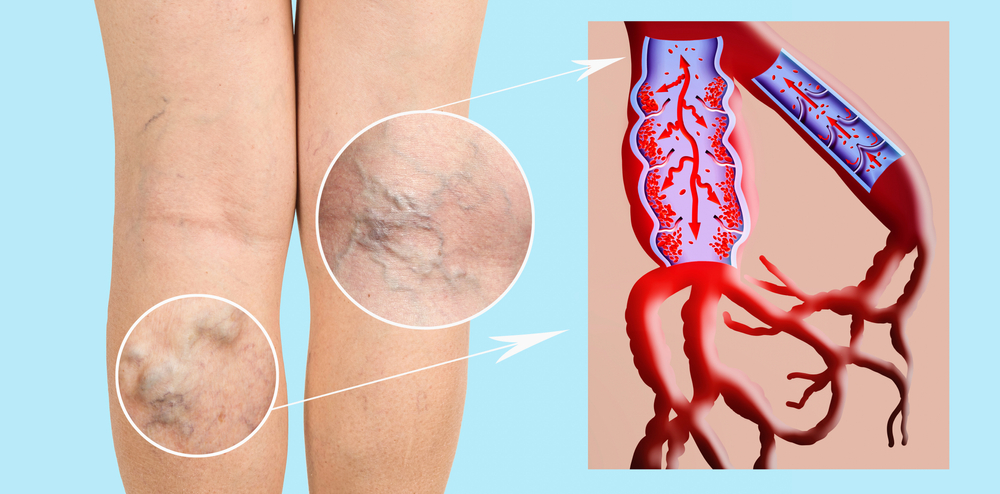
Varicose veins, the enlarged and twisted veins commonly seen on legs, are more than just a cosmetic concern. These veins can signal deeper health issues and sometimes lead to complications if left untreated. To better understand them, let’s decode the six key factors that contribute to their development, as well as the options available for managing them.
1. Genetics: Your Family History
One of the biggest predictors of varicose veins is your genetic makeup. If a close relative has varicose veins, your chances of developing them are significantly higher. Genetics influences vein wall strength, valve function, and the structure of your vascular system. Weak valves allow blood to backflow, causing veins to enlarge and appear more prominent. So, if you have a family history of varicose veins, take extra care in prevention and early management.
2. Age and Vein Health
As we age, our veins lose elasticity, which can lead to weakened valves and blood pooling in the legs. This is especially common for people over 50, though younger people can develop varicose veins too. Age-related deterioration in vein structure can lead to more frequent symptoms, including swelling, pain, and heaviness in the legs. Regular physical activity, maintaining a healthy weight, and a diet rich in nutrients can help support vein health as you age.
3. Gender Differences: Women at Greater Risk
Women are more likely to develop varicose veins than men. Hormonal fluctuations during menstruation, pregnancy, and menopause play a significant role, as female hormones tend to relax vein walls, making them more susceptible to varicosity. Additionally, hormonal therapies, including birth control pills, can increase the risk of vein issues due to the impact on blood flow and vein elasticity.
4. Lifestyle and Occupation: Standing and Sitting Matters
Occupations that involve prolonged standing or sitting can exacerbate varicose veins. When you stand or sit for extended periods, blood flow slows, increasing the likelihood of blood pooling in the lower extremities. Jobs in retail, healthcare, or office settings can contribute to vein issues if proper circulation breaks or movements aren’t incorporated throughout the day. Regularly moving your legs, stretching, and elevating your legs can help combat the effects of a sedentary or prolonged standing lifestyle.
5. Obesity and Varicose Veins
Carrying excess weight puts additional pressure on your veins, especially in the legs, making it harder for blood to flow back to the heart. This pressure weakens vein walls and valves, increasing the risk of varicose veins. Maintaining a healthy weight through balanced nutrition and regular exercise can relieve strain on the venous system and may prevent or reduce the severity of varicose veins.
6. Pregnancy and Vein Changes
Pregnancy increases blood volume and pressure on the veins, particularly in the pelvic area and legs. As the uterus expands, it puts pressure on the inferior vena cava (the vein responsible for returning blood from the lower body to the heart), contributing to vein enlargement. Hormonal shifts during pregnancy can also relax vein walls. While varicose veins related to pregnancy often improve after delivery, taking steps like elevating your legs, wearing compression stockings, and staying active can help manage symptoms.
Managing Varicose Veins: Treatment and Prevention
If you already have varicose veins, there are several management options available:
- Compression Stockings: Wearing these can help reduce pain and prevent further swelling by improving circulation.
- Lifestyle Changes: Regular exercise, weight management, and taking breaks from prolonged standing or sitting can prevent new varicose veins and ease existing symptoms.
- Medical Procedures: For more severe cases, minimally invasive treatments like sclerotherapy, laser therapy, and endovenous ablation may be recommended. These procedures target and close off affected veins, redirecting blood flow to healthier veins.
Conclusion
Understanding the factors behind varicose veins can empower you to take control of your vein health. While some factors like genetics and gender are out of your control, lifestyle adjustments and preventive measures can make a significant difference. Consulting a healthcare professional can help you determine the best course of action based on your individual risk factors and symptoms..